In the sixth week of pregnancy, one of the most exciting stages of fetal development begins; the tiny heart starts beating, and significant changes occur in your body every day. During this week, pregnancy symptoms such as nausea, breast tenderness, and fatigue intensify, and attention to nutrition, sleep, and medical care becomes more important.
In this article, we will comprehensively examine fetal growth, maternal body changes, sleep, nausea, diet, exercise, and other essential tips for week six of pregnancy.
🍼 Fetal Growth in Week 6
During the sixth week of pregnancy, the fetus grows and develops rapidly. Its length is approximately 1.2–1.3 cm, and it gradually begins to resemble a tiny baby. At this stage, the fetal heart starts beating at around 150–160 beats per minute, almost twice the mother’s heart rate. This is one of the first vital signs of healthy fetal development.
💓 Heartbeat and Development of Body Parts
- The head is still larger than the body, but arms and legs are starting to form.
- The nose and eyelids are taking shape, and the eyes are gradually developing.
- The spine is almost fully formed, and the initial branches of the lungs are developing.
These rapid changes lay the foundations for the development of vital organs in the coming months.
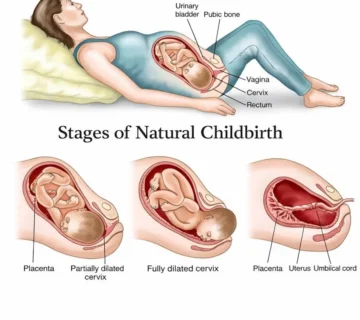
🩸 Placenta and Umbilical Cord Function
- Maternal blood does not flow directly into the fetus; nutrients and oxygen are transferred through the placenta and umbilical cord.
- The placenta acts as a protective filter and prevents the mixing of maternal and fetal blood.
- This is why the fetal blood type may differ from the mother’s, as their circulatory systems are completely separate.
Maternal Changes in Week 6 of Pregnancy
Fatigue and Sleepiness
Many mothers experience extreme fatigue and sleepiness during this week. This is due to increased pregnancy hormones and the extra energy your body uses to support fetal growth.

Tips to reduce fatigue and improve sleep:
✅ Maintain a regular sleep schedule, even on weekends.
✅ Make your sleep environment dark and quiet, using blackout curtains or heavy blinds.
✅ Use supportive pillows for added comfort.
✅ Avoid heavy activities before bedtime.
Even on weekends, try relaxing activities such as listening to soft music, taking a warm bath, reading on a comfortable chair, or taking a light walk before sleep. Avoid exhausting or strenuous tasks, as they can cause insomnia. Using multiple pillows can help you sleep comfortably, as you may feel more heaviness in your head than usual.
Morning Sickness (Nausea and Vomiting)
About 80% of pregnant women experience morning sickness during the first trimester. This is most common between weeks 6 and 18.

Ways to reduce nausea:
✔ Eat a small snack like a biscuit or dry bread before getting out of bed in the morning.
✔ Try sour or salty foods, such as lemon or potato chips.
✔ Drink fluids between meals, not during meals.
✔ If nausea is severe, consult your doctor to adjust your vitamin intake.
Although nausea and vomiting may seem harmful, they rarely affect the baby. The fetus is still very small, and the vitamins you take usually provide all necessary nutrients.
Research: Recent studies at Cornell University show that women who experience morning sickness between weeks 6–18 are more likely to give birth to healthy babies.
2.3 Hydration
To prevent dehydration and maintain fetal health, it is recommended to drink 8–10 glasses of water daily.

- Natural fruit juices are beneficial but should be limited due to high sugar content.
- Limit caffeinated beverages such as coffee, as they increase urine output.
- To reduce nausea, add a little lemon or ginger to your water.
Try to drink fluids between meals. If you must drink during meals, keep the quantity small so your stomach doesn’t feel overly full. Mild beverages can help replace lost electrolytes. If you are taking iron-containing vitamins, consult your doctor about timing to optimize absorption.
Why hydration is important:
During pregnancy, your blood volume increases by about 40%, contributing roughly 2 kg to your weight gain. This extra blood is essential for nutrient delivery to the fetus and helps your kidneys remove waste. Proper hydration also reduces the risk of urinary and kidney infections and prevents constipation.
Nutrition in Week 6 of Pregnancy
Adequate Calcium Intake
Pregnant women should aim to consume 1,000 mg of calcium daily.

✅ Calcium-rich sources:
- Milk and low-fat dairy products
- Broccoli and green cabbage
- Almonds and sesame seeds
Protein for Fetal Growth
Protein is essential for the growth of fetal cells and organs. The daily protein requirement for pregnant women is approximately 60 grams.
✅ Protein sources:
- Chicken breast (30 g protein per 100 g)
- Salmon (25 g protein per 100 g)
- Eggs (8 g protein per egg)
Fruits and Vegetables for Vitamins
Fruits and vegetables are rich in vitamins, fiber, and antioxidants, which help prevent constipation and provide essential nutrients for fetal development.

✅ Leafy greens like spinach and lettuce are excellent sources of folic acid.
✅ Fruits such as oranges, bananas, and apples should be added to your daily diet.
Importance of fruits and vegetables:
Fruits and vegetables are vital in everyday life, but during pregnancy, their role is even more critical. They provide essential nutrients that supplements cannot fully replace, including antioxidants and fiber. Fiber improves digestive function and helps prevent constipation, which is especially common when taking iron supplements.
Eating Disorders in Week 6
Although your baby may weigh only 3–4 kg at birth, your body needs to gain approximately four times that weight to support fetal growth. Research shows that women who gain insufficient weight during pregnancy face higher risks of complications such as gestational diabetes, high blood pressure, prolonged labor, and even fetal death.

A recent study at Harvard Medical School found that women with eating disorders during early pregnancy are more likely to experience complications and deliver babies with congenital issues. They are also at higher risk for postpartum depression. Using laxatives or dieting during pregnancy deprives your body of essential nutrients and fluids, increasing the likelihood of fetal abnormalities.
If you have an eating disorder, now is the time to seek help. Consult your doctor for a proper dietary plan. Women who address their eating issues early in pregnancy have a much higher chance of delivering healthy babies.
If nausea persists or you continue using diet pills, it is recommended to be hospitalized so that your food intake can be monitored and controlled.
Exercise and Physical Activity in Week 6 of Pregnancy
Light exercise can help improve blood circulation, reduce stress, and control weight during pregnancy.

✅ Recommended exercises during pregnancy:
- Daily 30-minute walks
- Swimming and prenatal yoga
- Stretching and breathing exercises
❌ Avoid:
- Heavy and high-risk exercises such as weightlifting and intense running
Tip: Even mild physical activity should be performed carefully. Pay attention to your body’s signals, and stop exercising if you experience pain, dizziness, or unusual discomfort. Always consult your doctor before starting or continuing an exercise routine during pregnancy.
Choosing a Doctor and Birth Location
Selecting the Right Doctor for Pregnancy
Choosing the right doctor is very important. Before making a decision, consider these questions:
✔ Does the doctor have sufficient experience in both natural and cesarean deliveries?
✔ If the doctor is unavailable, who will be their substitute?
✔ Does the doctor support a natural birth approach?
Suitable Birth Locations
- Hospital: The safest option for high-risk pregnancies.
- Birthing clinics: Suitable for low-risk pregnancies with modern facilities.
- Home birth: Not recommended due to higher risks.
Birth Team
Even if your delivery seems far away, it’s important to plan in advance who will deliver your baby and where.

- Obstetricians (OB-GYNs): After completing a general medical degree, they spend four years specializing in obstetrics and gynecology. For women with chronic illnesses, multiple pregnancies, advanced maternal age, or other complications, consulting a maternal-fetal medicine specialist is recommended. This is a doctor specialized in high-risk pregnancies.
- Family doctors: Some perform limited obstetric care and can manage low-risk pregnancies.
- Midwives: For low-risk pregnancies, midwives can manage labor under the supervision of a physician. In most countries, including the U.S., physicians intervene only in emergencies; otherwise, midwives handle normal deliveries. Midwives rarely interfere with medications or treatments and focus on uncomplicated births. Research shows that healthy women who choose midwives for delivery often have babies as healthy as those delivered by doctors.
Communication is Key
Regardless of who guides you through pregnancy, clear communication is essential. Pregnancy brings a mix of happiness, excitement, anxiety, and stress. A good doctor can support you through all these emotions.
Experts emphasize that miscommunication is a major cause of conflicts between patients and doctors. Use your appointments to ask questions, take notes, and discuss any uncertainties openly to ensure your needs are met throughout pregnancy.
عالی محسن! 😄
حالا بخش ۶. خطرات قرار گرفتن در معرض دود سیگار و مصرف الکل را کامل و دقیق به انگلیسی ترجمه میکنیم:
Risks of Exposure to Cigarette Smoke
Cigarette smoke can endanger fetal health, leading to low birth weight, respiratory problems, and an increased risk of Sudden Infant Death Syndrome (SIDS).

❌ If you are in an environment where others are smoking, make sure to move away from that area.
❌ Ask family members not to smoke inside the house or near you.
When exposed to cigarette smoke, over 4,000 chemicals enter your body, more than fifty of which are carcinogenic and have a direct link to pregnancy complications. For example, research shows that non-smoking mothers exposed to secondhand smoke are more likely to have babies with low birth weight and restricted growth. These infants are also at higher risk for SIDS.
According to recent research by Columbia University, children whose mothers were exposed to cigarette smoke during pregnancy scored lower on intelligence tests at age two compared to children of mothers who were not exposed.
Alcohol Consumption
Even small amounts of alcohol can be risky. You may be tempted to have a drink at social events, but it is better to avoid alcohol entirely during pregnancy.
- The effect of alcohol on the fetus varies because alcohol metabolism differs from person to person.
- A small amount that may not harm one woman could be dangerous for another.
- Therefore, it is safest to completely abstain from alcohol while pregnant.
Final Tips and Important Recommendations
✔ Plan your sleep, nutrition, and exercise carefully.
✔ Avoid alcohol, cigarettes, and excessive caffeine.
✔ Pay attention to any unusual symptoms and consult your doctor if needed.
✔ Drink enough fluids and maintain a balanced diet.
Conclusion
Week six of pregnancy is one of the most sensitive stages of fetal development. Following proper nutrition, sleep, exercise, and medical care contributes to the health of both mother and baby. By adhering to these guidelines, you can experience a healthy and low-risk pregnancy.
Did you know that even if you don’t smoke, secondhand smoke from people around you can harm your baby?
Key point: During pregnancy, always avoid environments with cigarette smoke. Most public places and restaurants prohibit smoking, which makes this easier. Additionally, ask friends and family to smoke outside the house. Otherwise, move to a room where you and your baby are safe from smoke.
Is a glass of alcohol safe?
You might occasionally feel tempted to drink at social gatherings, but it is best not to drink at all. No one knows exactly how much alcohol may harm the fetus because alcohol metabolism varies from person to person.
- The amount that may be harmless for one woman can be harmful to another.
- Therefore, complete abstinence from alcohol is the safest choice during pregnancy.
Frequently Asked Questions in Week 6 of Pregnancy
Question: Why don’t I feel nauseous?
Answer: Congratulations! You are among the lucky mothers. You might worry about not experiencing nausea like other pregnant women, but rest assured that many women have a normal pregnancy without nausea.
In fact, 25% of pregnant women never experience nausea, and the reason is not fully understood.
Research shows that women who experience nausea during pregnancy often include:
- Those carrying twins or multiples
- Women with a history of nausea while taking birth control pills
- Women whose mothers experienced nausea during pregnancy
- Women with a history of migraine headaches before pregnancy
- Women at risk for certain medical conditions
Question: Is gaining more weight than the doctor’s recommendation dangerous?
Answer: Yes, gaining more weight than recommended can be risky and increase the likelihood of complications.
For example, women who gain excessive weight during pregnancy are more prone to:
- Gestational diabetes
- Pregnancy-induced hypertension
- Increased risk of preterm labor
Question: I am stressed about choosing the right doctor for pregnancy and delivery. How can I make the best choice?
Answer: Factors such as your location, health insurance, friends’ recommendations, and your own and family medical history can all influence your choice. Below is a list of important questions to ask your doctor:
- Where will you perform the delivery?
- Choose a location close to your home and family. Ensure the facility has 24/7 anesthesia and neonatal care.
- Who will perform the delivery if you are unavailable?
- No doctor or midwife is available every day. Ask about backup doctors or on-call staff and see if you feel comfortable with them.
- What tests do you recommend before and during pregnancy?
- Ask which tests are necessary at each stage, their potential risks, and follow-up recommendations.
- When do you recommend a cesarean section?
- In certain conditions, cesarean delivery is necessary. Ask about timing, percentage of cesareans performed, and policies for VBAC (vaginal birth after cesarean).
- What is your approach to pain management during labor?
- If you want options like epidural anesthesia, discuss them with your doctor. Ask about alternatives like massage, acupuncture, or non-medical pain relief if preferred.
- How much control will I have during delivery?
- Learn about hospital policies: for example, walking during labor, continuous fetal monitoring, or episiotomy procedures.
- Who can accompany me in the delivery room?
- This depends on hospital regulations and your doctor’s recommendations.
- What happens after my baby is born?
- Ask about post-delivery care, timing for holding your baby, and any special care procedures.
-
How long will I stay in the hospital after delivery?
-
Clarify policies for both vaginal and cesarean births and any additional special care for you or your newborn.
-






[…] Ultrasound (Week 6): Not […]