The first days after childbirth, medically referred to as the Postpartum problems period, represent one of the most sensitive and formative stages in a woman’s life. From the moment the baby is born, the body and mind of a new mother enter an entirely new phase—one characterized by significant hormonal, physical, and psychological changes that require awareness and special care.
During this period, a mother may experience a range of challenges, including pain, postpartum bleeding, profound fatigue, mood fluctuations, and concerns related to breastfeeding. Alongside these difficulties, however, profound maternal emotions and the emotional bonding between mother and newborn begin to develop. Becoming familiar with what is considered normal and recognizing warning signs during the postpartum period can help mothers navigate these days with greater confidence, calm, and reassurance.
In this article, we provide a clear and evidence-based overview of what the postpartum period entails, the common problems mothers may face in the early days after childbirth, and the essential measures required to protect both physical and mental health during this critical time.
How to Introduce an Older Sibling to a Newborn Baby
After the postpartum period and the birth of a new baby, one of the most common concerns for parents is the reaction of the older child or children. An older sibling may experience feelings of jealousy, fear of being replaced, or emotional confusion. For this reason, the way the first encounter between the older child and the newborn is managed plays a crucial role in shaping their future emotional bond.

The First Meeting of the Older Child and the Newborn in the Hospital
If your older child is planning to visit you in the hospital, it is advisable to have the newborn placed in the nursery for a short period before the child enters the room. This recommendation also applies when rooming-in is practiced and the newborn usually stays in the mother’s room. Doing so helps prevent the older child from feeling that all of the mother’s attention has been immediately taken away by the new baby.
Creating a Sense of Security for the Older Child
When the older child enters the room:
-
Begin by holding them in your arms and offering warmth, affection, and undivided attention.
-
Allow the child to explore gifts, flowers, or parts of the hospital bed that may interest them.
These simple actions reassure the child that they continue to hold a special and secure place in the family.
Involving the Older Child in Bringing the Newborn
Once the older child feels calm and reassured, you may accompany them—together with your partner—to the nursery so they can participate in bringing the newborn back to your room. Even small tasks, such as helping to push the baby’s bassinet, can foster a sense of responsibility, importance, and inclusion.
At the end of the visiting time, you may also ask the older child to help return the newborn to the nursery. This simple form of involvement can significantly reduce feelings of jealousy and strengthen the emotional bond between siblings from the very beginning.
Appropriate Nutrition in the First Days After Childbirth
After the postpartum period begins, a mother’s body enters a phase of recovery and regeneration. Childbirth—whether vaginal or via cesarean section—is an extremely energy-demanding event, and it is entirely normal for a new mother to experience intense hunger shortly after delivery. In effect, childbirth is comparable to a physical marathon, during which a significant portion of the body’s energy reserves is depleted.

Contrary to what many mothers expect, a full or substantial meal is not always provided immediately after delivery in the labor or delivery room. For this reason, it is advisable to prepare in advance by bringing simple, nutritious snacks or arranging for food to be brought from outside the hospital.
First Priority: Replacing Lost Calories
When choosing foods in the first days after childbirth, adequate caloric intake is essential. The body expends a large amount of energy during labor and now requires prompt replenishment. At this stage, undereating is not recommended; in most cases, eating more is preferable to eating less.
Nutrition for Breastfeeding Mothers: Increased Caloric Needs
If you are breastfeeding, it is important to know that breast milk production requires approximately 500 additional calories per day. Therefore:
-
Include foods from all major food groups
-
Pay attention to your body’s natural appetite
-
Avoid unnecessary dietary restrictions or skipped meals
Protein: Essential for Postpartum Recovery
After childbirth, the body needs sufficient protein to repair tissues, rebuild muscles, and promote wound healing. Suitable protein sources include:
-
Milk and yogurt
-
Porridge or semolina-based foods
-
Eggs
-
Meat, poultry, and legumes
Breastfeeding mothers are generally advised to consume at least five glasses of milk or equivalent dairy products daily to meet their own nutritional needs and support adequate milk quality.
Fiber Intake to Prevent Postpartum Constipation
One of the most common problems in the early postpartum period is constipation. During labor and in the days following delivery, gastrointestinal motility often slows, and it may take several days for normal bowel function to return.
To help prevent or relieve constipation:
-
Consume fresh fruits regularly
-
Include salads and vegetables in daily meals
-
Avoid low-fiber diets during this period
Fluid Intake: Essential for New Mothers
Adequate hydration is particularly critical in the first days after childbirth, especially for breastfeeding mothers. It is recommended to:
-
Drink at least 12 glasses of fluids per day
-
Prefer non-caffeinated beverages
Sufficient fluid intake helps to:
-
Soften stools and reduce constipation
-
Prevent urinary tract infections
-
Support the production and maintenance of breast milk volume
Sleep: The First and Most Important Need in the Early Days After Childbirth
In the first days after the postpartum period, sleep should be one of your highest priorities. While in the hospital, try to rest whenever the opportunity arises; even short or fragmented periods of sleep are extremely valuable for physical recovery. The reality is that in the months—and sometimes years—ahead, uninterrupted nighttime sleep may not be easily achievable. Therefore, it is especially important to rest as much as possible during these early days.

Sleep deprivation during this period can worsen fatigue, contribute to mood fluctuations, and reduce physical stamina. In contrast, adequate rest supports faster physical recovery and helps the body adapt more smoothly to the demands of motherhood.
Feelings of Weakness and Exhaustion After Childbirth Are Normal
Many mothers, particularly those who have experienced prolonged labor, report profound weakness and exhaustion after delivery. In these situations, one or two nights of inadequate sleep combined with intense physical exertion can leave the body feeling severely depleted. Some women describe this sensation as feeling deeply bruised or physically overwhelmed, similar to having experienced a major accident.
Shivering, Muscle Pain, and Severe Fatigue Are Not Cause for Alarm
In the first hours after childbirth, you may:
-
Experience shivering or trembling
-
Feel soreness in muscles you were previously unaware of
-
Feel uncertain about your ability to walk or even reach the bathroom
These symptoms are commonly reported by women who have just given birth and typically result from a combination of extreme fatigue, hormonal fluctuations, and the sudden release of physical strain following delivery.
Why Is It Difficult to Sleep Despite Extreme Fatigue?
A common concern among new mothers is the inability to fall asleep despite overwhelming tiredness. This phenomenon often occurs due to elevated adrenaline levels in the body after childbirth. In addition, factors such as:
-
Intense hunger
-
Anxiety about caring for the newborn after discharge
-
Emotional excitement following the birth
can further interfere with the ability to sleep. It is important to understand that all of these responses are normal and, in most cases, gradually subside within the first one to two days after delivery, requiring no cause for concern.
Psychological and Emotional Challenges After Childbirth: From Normal Sadness to Depression
The early days after childbirth affect not only a mother’s physical health but also her mental and emotional well-being. A new mother’s psychological state is influenced by significant hormonal changes, physical exhaustion, sleep deprivation, and the responsibilities associated with caring for a newborn. As a result, many women experience emotions that may feel unfamiliar or unexpected.

Feelings such as sadness, unexplained crying, irritability, anxiety, low motivation, or even guilt are very common and often normal in the days following childbirth. This condition, known as postpartum blues (Baby Blues), typically:
-
Begins within the first few days after delivery
-
Gradually improves within 1 to 2 weeks
-
Does not require medical treatment
The Difference Between Postpartum Blues and Postpartum Depression
If these emotional symptoms:
-
Persist for more than two weeks,
-
Become more intense, or
-
Interfere with the mother’s ability to care for herself or her baby,
they may indicate postpartum depression, a condition that requires medical attention and, in some cases, specialized treatment.
Warning signs include:
-
Persistent feelings of hopelessness
-
Complete loss of interest in the newborn
-
Thoughts of self-harm or harm toward the baby
-
Severe anxiety or panic attacks
These symptoms should never be ignored. Seeking help from a gynecologist, obstetrician, or mental health professional is not a sign of weakness—it is an essential part of appropriate and responsible postpartum care.
Seek Support From Those Around You; You Are Not Expected to Do Everything Alone
In the first days after the postpartum period, one of the most important factors contributing to faster recovery is making appropriate use of support from family members and healthcare professionals. Severe fatigue, sleep deprivation, and physical and emotional strain after childbirth are entirely normal, and you are not expected to go through this phase on your own.

The Role of Nurses in Caring for a New Mother
In the hospital setting, nurses are among your most important sources of support. Be sure to communicate openly with your nurse and let them know if you experienced significant sleep deprivation during labor and are feeling extremely exhausted. You may request to be awakened only for breastfeeding so that you can rest adequately during other hours.
What Care Do Nurses Provide After Childbirth?
Nurses are responsible for closely monitoring the overall condition of a new mother. This care includes:
-
Measuring blood pressure
-
Monitoring heart rate
-
Checking body temperature
Any abnormal change in these vital signs may indicate the onset of infection or excessive bleeding, making early detection critically important.
In addition to monitoring vital signs, postpartum nursing care also includes:
-
Assessing the normal progression of physical recovery
-
Assisting with the initiation and continuation of breastfeeding
-
Evaluating the healing of sutures
-
Assessing uterine firmness and involution (which may require uterine massage in some cases)
Why Do Nurses Emphasize Urination After Childbirth?
One aspect of postpartum care that may feel uncomfortable for some mothers is the nurses’ insistence on regular urination. Even if you feel reluctant, it is important to understand that urination after childbirth is medically essential.
If a mother is unable to urinate:
-
The bladder may become overdistended
-
The uterus may not contract effectively
-
The risk of bleeding and serious complications increases
For this reason, even if the process feels unpleasant, cooperating with nursing staff regarding urination plays a vital role in protecting your health during the postpartum period.
The First Trip to the Bathroom After Childbirth: A Worrisome but Normal Experience
For many mothers, the first bathroom visit in the early days after childbirth is one of the most anxiety-provoking experiences. This concern is entirely natural and is often related to pain, burning sensations, or fear of injury to the genital area or stitches. However, understanding what is normal and knowing how to make this process more comfortable can significantly reduce anxiety.

The First Urination After Childbirth: Why Can It Be Painful?
The first urination after childbirth may:
-
Be completely normal and painless, or
-
Be accompanied by noticeable burning or discomfort
This discomfort is most commonly caused by:
-
Temporary irritation or minor injury to the urethra during delivery
-
Pressure and swelling in surrounding tissues
-
The presence of perineal stitches
In some mothers, fear of pain or concern about injury to the perineal area may make urination feel temporarily difficult or even impossible.
A Simple Method to Reduce Burning During Urination
One effective and safe way to reduce burning during urination after childbirth is to pour cool or lukewarm water over the genital area while urinating. This method:
-
Helps relieve the burning sensation
-
Soothes local irritation
-
Allows the mother to get through this stage with greater comfort and calm
The First Bowel Movement After Childbirth: Why Is It Difficult?
The first bowel movement after childbirth can also be a stressful experience. During delivery:
-
The pelvic floor muscles become stretched and relaxed
-
The strength needed to bear down is temporarily reduced
At the same time, the need to apply pressure—especially when stitches are present—can feel painful and concerning. As a result, many mothers feel fear or hesitation at this stage. It is important to know, however, that this condition is temporary and manageable.
Why Is Urination After Childbirth So Important?
Once you are able to urinate successfully for the first time and the nursing staff’s concerns are resolved, you are usually monitored less frequently until hospital discharge. This highlights the fact that regular urination after childbirth is an important indicator of postpartum recovery and plays a key role in reducing the risk of complications after delivery.
After Childbirth: Do Not Feel Embarrassed—Ask Questions and Request the Support You Need
In the first days after the postpartum period, many mothers hesitate to express their needs due to exhaustion, pain, or feelings of embarrassment. However, making use of hospital postpartum care resources plays an important role in reducing pain and preventing infection. Remember that asking questions and requesting assistance is an essential part of proper care for a new mother.

Hygiene and Postpartum Care Supplies in the Hospital
After being transferred to the postpartum ward, you are usually provided with supplies such as:
-
Ice packs
-
Postpartum sanitary pads
-
A perineal cleansing spray or rinse bottle
The cleansing spray can be used when going to the bathroom and even during urination with warm water to reduce burning and discomfort—especially if the odor of urine is bothersome.
If an ice pack is not provided, be sure to ask your nurse. During the first few days after childbirth, ice therapy is one of the most effective ways to reduce pain and swelling in the perineal area.
Flexible Ice Packs: A Simple and Effective Tip
A very practical alternative to standard ice packs is the use of hospital gloves filled with ice. These improvised ice packs:
-
Stay colder
-
Are more flexible
-
Conform better to the shape of the body
You may ask the nurse to provide one or two gloves and refill them with ice as needed throughout the day.
Warm Sitz Baths: Promoting Faster Healing
Ask your nurse for a plastic sitz bath basin. It is recommended to:
-
Use it several times a day
-
Sit in warm water for at least 15 minutes each time
Warm sitz baths:
-
Promote a sense of relaxation
-
Help reduce pain and muscle spasm
-
Improve local blood circulation
-
Lower the risk of infection
-
Accelerate the healing of perineal stitches
The same type of basin can also be used at home after discharge.
Prepared Pads and Witch Hazel: Effective Relief for Perineal Pain
Pads soaked in witch hazel extract (Witch Hazel) are an effective method for reducing swelling and pain in the perineal area. You may:
-
Request a bottle of witch hazel from the nursing staff
-
Soak a pad or gauze in the solution and place it on a sanitary pad
-
Or place the soaked pad directly on an ice pack for enhanced relief
If the pain is severe, you may ask the nurse for a topical anesthetic spray or foam and apply an appropriate amount to the sanitary pad.
Using Frozen Pads at Home
If pain persists after returning home:
-
Pour witch hazel onto several sanitary pads
-
Moisten them thoroughly (without fully soaking them)
-
Place them in the freezer
Many mothers report that these frozen pads provide exceptional relief for perineal pain and inflammation. Alternatively, square gauze pads soaked in witch hazel can be stored in the refrigerator for later use.
Yes, Pain After Childbirth Is Real — but It Is Expected and Manageable
The reality is that childbirth is not a painless process. The passage of a newborn through the birth canal places significant pressure on surrounding tissues, and it is entirely normal for a mother’s body to experience pain and sensitivity after delivery. Experiencing pain after childbirth does not indicate a problem; rather, it is a natural part of the body’s healing and recovery process.

Pain Caused by Tearing or Episiotomy
During vaginal delivery, the following may occur:
-
Natural tearing of the vaginal tissues, or
-
An episiotomy, a controlled incision made by the obstetrician to facilitate delivery
In both cases, sutures are placed in the perineal area after birth, which may lead to:
-
A sensation of tightness
-
Localized pain
-
Discomfort when sitting or moving
These symptoms typically improve gradually over the days and weeks following childbirth.
Unexpected Sources of Pain After Childbirth
Even when delivery occurs without stitches, a mother may still experience:
-
Minor abrasions or inflammation of the labia
-
Pain in unexpected areas such as the thigh muscles (especially if labor occurred in an upright position)
-
Chest muscle soreness due to repeated bearing down
-
Or even hemorrhoids
These discomforts are generally temporary and tend to resolve with appropriate postpartum care.
A Sensation of Pelvic Heaviness or Pressure — Why Does It Occur?
Some mothers report a feeling of heaviness or pressure in the pelvic region or internal organs after childbirth. This sensation may be unfamiliar and somewhat concerning at first. It is most commonly caused by:
-
Stretching of the pelvic floor muscles
-
Sudden anatomical changes following the delivery of the baby
In most cases, as pelvic floor strength gradually returns, this sensation diminishes or resolves completely over time.
Importantly, many mothers find that this feeling becomes less noticeable or is eventually perceived as a normal part of the postpartum recovery period.
Hemorrhoids After Childbirth: Common, Uncomfortable, but Treatable
Hemorrhoids are one of the common postpartum problems experienced by new mothers. Hemorrhoids refer to the swelling of veins around the anal area and are typically caused by sustained pressure—such as the weight of the fetus during pregnancy or intense straining during labor.
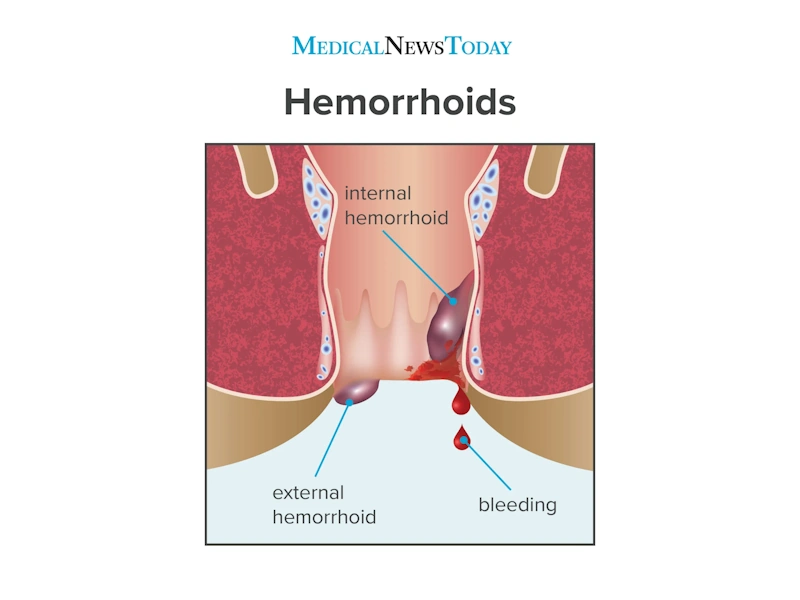
Many women who have recently given birth experience some degree of hemorrhoids, and fortunately, in most cases this condition is temporary and gradually resolves. However, while hemorrhoids are active, sitting or having a bowel movement can be particularly uncomfortable and painful.
How to Reduce Constipation and Support Hemorrhoid Recovery
Constipation is a major factor that can worsen postpartum hemorrhoids. To prevent and relieve constipation, the following measures are recommended:
-
Ensure adequate fluid intake
-
Engage in gentle daily walking
-
Include fresh fruits and vegetables in your diet
-
Use mild stool softeners or laxatives if necessary, under the guidance of a healthcare provider
Sitting in Warm Water: A Simple and Effective Method
Sitting in a warm bath or a plastic basin filled with warm water several times a day—each session lasting about 10 to 15 minutes—can:
-
Reduce pain and inflammation
-
Improve local blood circulation
-
Accelerate the healing process
This approach is one of the simplest and most effective ways to relieve hemorrhoid symptoms after childbirth.
Proper Sitting Techniques to Reduce Hemorrhoid Pain
To minimize pressure while sitting:
-
Use donut-shaped or hollow cushions
-
These cushions reduce direct pressure on the anal area
When leaving home, you may carry the cushion in a suitable bag to avoid prolonged standing or sitting on hard surfaces.
Topical Treatments for Postpartum Hemorrhoid Relief
Several simple and accessible treatments can help reduce hemorrhoid pain and swelling, including:
-
Multi-layer pads or gauze soaked in witch hazel extract (Witch Hazel)
-
Short-term use of hydrocortisone ointment at appropriate doses
These treatments often provide significant symptom relief and help mothers navigate this period more comfortably.
Physical Changes in a Mother’s Body After Childbirth: What Is Considered Normal?
After childbirth, many mothers become concerned when they notice changes in their bodies. It is important to remember that the body undergoes significant changes over the course of nine months, and returning to its pre-pregnancy state takes time.
Common Physical Changes After Childbirth
During the first weeks and months after delivery, the following changes may be observed:
-
A soft or loose abdomen with some remaining protrusion
-
Gradual weight loss rather than rapid or sudden reduction
-
Weakness or laxity of the pelvic floor muscles
-
Skin changes such as darkening or stretch marks
-
Temporary abdominal sagging and a sensation of pelvic heaviness
In most cases, these changes are normal and reversible. With:
-
Time
-
Proper nutrition
-
Gradual physical activity
-
Appropriate postpartum exercises
the body typically recovers progressively.
When Should Physical Changes Be a Cause for Concern?
If symptoms such as the following are present:
-
Severe or persistent pelvic organ prolapse
-
Ongoing urinary leakage
-
Intense or long-lasting pain
-
Little to no improvement after several months
a specialized evaluation by a physician or pelvic floor physical therapist is recommended.
Physical Realities in the First Days After Childbirth: Understanding Common Sources of Pain
The first days after the postpartum period are accompanied by physical changes and sensations that, when understood, can reduce fear and support better decision-making. Many of these pains and symptoms—although uncomfortable—are normal and temporary.
Tailbone Pain After Childbirth: More Common Than You Might Expect
Some mothers experience tailbone (coccyx) pain after childbirth, particularly following a vaginal delivery. This discomfort may result from:
-
Intense pressure during the passage of the baby
-
Bruising or stretching of surrounding ligaments
-
In rare cases, a mild displacement of the coccyx
In most instances, this pain gradually improves over several weeks—often within about a month—and is generally not a cause for concern.
Afterpains: Uterine Contractions That Help the Uterus Shrink
After childbirth, the uterus undergoes intermittent contractions as it returns to its normal, pre-pregnancy size.

These contractions:
-
Are usually milder during a first delivery
-
Can be more intense and uncomfortable in subsequent births
Common Pain Medications for Afterpains
To manage afterpains, medications such as:
-
Acetaminophen (Paracetamol)
-
Ibuprofen
are commonly used and are considered safe and effective when taken at appropriate doses.
In certain cases, a physician may prescribe stronger pain medications. However, it is important to note that:
-
Opioid medications may cause dizziness, nausea, vomiting, and constipation
-
If you are breastfeeding, any pain medication should be taken only under the guidance of your obstetrician or gynecologist
Postpartum Bleeding: Normal, but With Limits
Relatively heavy bleeding after childbirth is normal. However, the amount and duration of bleeding should be carefully monitored.
🔴 If, three hours after delivery, you find that:
-
You need to change a postpartum sanitary pad every hour
you should immediately inform your nurse or, if you are at home, contact your physician or midwife.
You may also notice:
-
Bruising or discoloration on the face or chest
This is usually caused by intense pushing during labor and is generally not a cause for concern.
Sweating and Unusual Symptoms After Childbirth: Why Do They Occur?
After delivery, the body works to eliminate excess fluids accumulated during pregnancy. As a result:
-
Heavy sweating, especially at night, is common
-
Some mothers may experience hives or itchy skin rashes
Although the exact cause of these symptoms is not always clear, fortunately:
-
They usually resolve on their own
-
In most cases, they are not dangerous
⚠️ Warning Signs That May Indicate a Serious Infection
If you experience any of the following symptoms, you should contact your obstetrician or gynecologist immediately:
-
A fever higher than 37.9°C (100.2°F) measured orally
-
Passage of blood clots larger than the size of a walnut
-
Foul-smelling vaginal discharge
-
Pain during urination that worsens instead of improving
-
Pain in the thigh or calf without visible redness or swelling
-
Pain, redness, or tenderness in the breast
-
Severe or persistent shivering after childbirth
⚠️ Reputable medical sources also emphasize that the presence of these symptoms after childbirth requires prompt evaluation. For example, the Mayo Clinic’s postpartum care guidelines clearly outline these warning signs.
Shivering After Childbirth: Common but Worth Noticing
Shivering may occur after both vaginal and cesarean deliveries. This condition is usually caused by:
-
Significant physiological stress
-
Blood loss
-
The body’s nervous system readjusting after delivery
In most cases, postpartum shivering resolves spontaneously.
Easier Breathing After Childbirth: The Role of Massage
Some mothers—particularly after difficult or prolonged labor—experience shortness of breath or a sensation of tightness in the chest following childbirth.

In many cases, this occurs due to:
-
Muscle spasms and tension in the chest wall
-
Prolonged physical strain during labor
Postpartum Massage: A Genuine Therapeutic Aid
Specialized postpartum massage can:
-
Restore normal breathing patterns
-
Reduce muscle tension in the thighs and pelvic region
-
Alleviate persistent pain and improve sleep quality
For this reason, many physicians recommend postpartum massage—performed by a trained professional—as early as it is safely possible. Warm showers may also provide additional relief.
Some massage therapists specialize specifically in prenatal and postpartum massage. Be sure to inquire about proper training and experience before choosing a provider.
Sexual Activity After Childbirth: When Is It Safe and What Should Be Considered?
One of the most common questions among new mothers (and sometimes fathers) is when sexual activity after childbirth is safe. There is no single answer that applies to everyone, as the appropriate timing depends on the mother’s physical recovery and emotional readiness.

In general, most physicians recommend:
-
Waiting at least 4 to 6 weeks after childbirth
-
Ensuring that postpartum bleeding has significantly decreased
-
Allowing sufficient time for stitches to heal
-
Confirming that the mother feels physically and emotionally prepared
Why Can Sexual Intercourse Be Painful After Childbirth?
During the first weeks postpartum, several factors may contribute to pain or reduced desire for sexual activity, including:
-
Vaginal dryness due to decreased estrogen levels, particularly in breastfeeding mothers
-
Discomfort or pain from stitches
-
Weakness of the pelvic floor muscles
-
Fatigue and sleep deprivation
These issues are common and usually improve over time with pelvic floor exercises (such as Kegel exercises) and the use of appropriate vaginal lubricants.
It is important to note that there is no obligation to resume sexual activity early. Open communication with one’s partner and attentiveness to the mother’s physical and emotional needs play a key role in maintaining a healthy and supportive relationship during the postpartum period.
Exercise in the First Days After Childbirth: Gentle, Early, and Appropriate
After nine months of pregnancy, the idea of exercise may not sound appealing to a new mother. However, gentle and well-planned movement is one of the most important factors in promoting faster physical recovery after childbirth. Notably, some simple exercises can be started even before leaving the delivery bed.
In the early hours after delivery, you may feel as though you have little or no control over your muscles—or may not even be aware of them at all. This is completely normal. Repeating simple movements every few hours helps gradually restore muscle responsiveness.
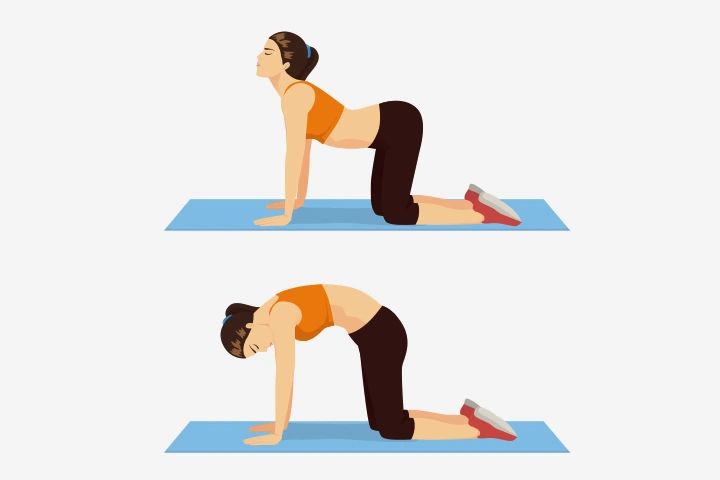
Kegel Exercises: The Foundation of Postpartum Exercise
Kegel exercises are among the most important and safest forms of exercise in the early postpartum period, as they directly target the pelvic floor muscles.
How to Perform Kegel Exercises
-
Contract the muscles surrounding the urethra, vagina, and anus
-
Hold the contraction for 3 seconds
-
Then fully relax the muscles
The easiest way to identify the correct muscles is to try stopping the flow of urine during urination. If the flow stops with muscle contraction, the exercise is being performed correctly.
Frequency and Repetitions
-
Twice daily
-
20 repetitions per session
Benefits of Kegel Exercises After Childbirth
Kegel exercises:
-
Increase blood flow to the vaginal area
-
Promote faster healing and strengthening of the pelvic floor muscles
-
Help prevent urinary leakage when laughing or sneezing
-
Play an important role in improving sexual function in the future
Walking After Childbirth: Uncomfortable but Essential
As soon as you are able, try to get out of bed and start walking. Even short, slow walks provide important benefits, including:
-
Activation of the circulatory system
-
Improved gastrointestinal function, which often slows after childbirth
-
Prevention of blood clot formation
-
Faster recovery of muscles and joints
Many mothers experience significant discomfort during their first attempts at walking. This is often described as a sensation of heaviness, pelvic pressure, or weakness in the legs and abdomen. These sensations are normal and typically lessen gradually with continued gentle movement.
Move Even When You Do Not Feel Like It

You may feel reluctant to walk or move at first, but it is important to understand that early, controlled movement is one of the key factors in optimal postpartum recovery. Start slowly, listen carefully to your body, and consult your physician or nurse if you experience severe or unusual pain.
Mothers After Cesarean Delivery: What You Should Know in the First Days
Mothers who deliver their baby by cesarean section generally do not experience pain related to perineal tearing or stitches. However, if attempts at vaginal delivery were made before the final decision to proceed with a cesarean section, some degree of perineal discomfort may still be present.
Nevertheless, cesarean delivery has its own specific challenges during the first days after childbirth.

Incision Pain and the Role of Post-Cesarean Bloating
The primary source of pain after a cesarean section is the abdominal incision, which involves both skin and underlying muscles. This pain may feel more intense due to:
-
Reduced gastrointestinal activity
-
The effects of anesthesia and pain medications
-
Gas accumulation and abdominal bloating
Bloating after a cesarean section is very common and can cause significant pressure and discomfort in the abdomen.
Some mothers report unexpectedly strong and frequent passage of gas during the first days after surgery. While this may feel alarming, it is normal and temporary and indicates the gradual return of bowel function.
Ways to Reduce Bloating and Pain After Cesarean Delivery
To reduce bloating and support faster recovery:
-
Get out of bed and begin walking gently as soon as possible
-
Short walks in the hospital corridor help stimulate bowel activity
-
Avoid putting excessive strain on your body and increase activity gradually
One simple and effective technique is to press a small pillow or cushion against the incision site when getting out of bed or moving. This method:
-
Reduces the sensation of pulling
-
Lessens pain during position changes
-
Provides a greater sense of control and stability
Rest and Accepting Help: The Key to Recovery After Cesarean Section
Recovery after a cesarean section depends largely on adequate rest and accepting help from others. The experiences of many mothers who have undergone multiple cesarean deliveries show that:
-
Trying to do everything independently can slow the healing process
-
The more rest you allow yourself during the first weeks, the better and faster your body will recover
During this period, seek support from your partner, family members, or caregivers, and allow your primary focus to remain on healing and caring for your newborn.
Frequently Asked Questions About Postpartum Problems (FAQ)
❓ Is pain after childbirth normal?
Yes. Experiencing pain, tightness, or discomfort in the first days after childbirth is completely normal. This pain may result from uterine contractions, stitches, muscle stretching, or the physical strain of labor, and it usually decreases gradually over time.
❓ How long is postpartum bleeding considered normal?
Postpartum bleeding typically lasts for several weeks and gradually becomes lighter. However, if you need to change a sanitary pad every hour or pass large blood clots, you should contact your physician or midwife immediately.
❓ Is constipation after childbirth normal?
Yes. Constipation is a common postpartum issue caused by reduced bowel activity, fear of pain, and the use of certain medications. Adequate fluid intake, dietary fiber, gentle movement, and mild stool softeners (if needed) can help relieve this condition.
❓ Do hemorrhoids after childbirth resolve on their own?
In most cases, yes. Postpartum hemorrhoids are usually temporary and tend to improve gradually with constipation relief, warm sitz baths, and appropriate topical treatments.
❓ When is it safe to resume sexual activity after childbirth?
In most cases, physicians recommend waiting at least 4 to 6 weeks after childbirth, once bleeding has decreased and stitches have healed. The mother’s physical and emotional readiness is a key factor in this decision.
❓ When can exercise be started after childbirth?
Light activities such as Kegel exercises and gentle walking can be started even in the first days after childbirth. More intense exercise should be introduced gradually and only with medical guidance.
❓ Is it normal to feel sad or cry after childbirth?
Yes. Many mothers experience mood swings and unexplained crying in the early postpartum period, which is usually temporary. However, if these feelings become severe or persistent, medical consultation is recommended.
❓ Which postpartum symptoms are considered dangerous?
High fever, foul-smelling discharge, heavy bleeding, severe or persistent pain, calf pain, or breast redness may indicate a serious condition and require immediate medical evaluation.
❓ How long does full physical recovery after childbirth take?
Returning to pre-pregnancy physical condition takes time and may require several months. Proper nutrition, sufficient rest, gradual physical activity, and patience play an important role in this recovery process.
Final Summary of Postpartum Challenges: Navigating the First Days After Childbirth Safely and Confidently
The first days after childbirth—medically referred to as the postpartum period—represent one of the most sensitive stages in a mother’s life. During this time, both the body and mind are simultaneously adapting to new conditions. This transition may involve pain, fatigue, emotional changes, anxiety, and at the same time, profound maternal emotions and bonding experiences.
Many of the challenges a new mother encounters during this period—such as pain, bleeding, constipation, hemorrhoids, mood fluctuations, sleep disturbances, and physical weakness—are normal and temporary. Understanding these changes and knowing which symptoms are expected versus which require medical evaluation play a crucial role in reducing anxiety and preventing complications.
During this period, the following measures are especially important:
-
Adequate rest
-
Proper nutrition and sufficient fluid intake
-
Gentle physical activity and simple exercises such as Kegel exercises
-
Accepting support from family members and healthcare providers
-
Paying close attention to one’s physical and emotional needs
All of these contribute significantly to a faster and healthier recovery.
It is also essential to remember that every mother’s experience is unique. Comparing oneself to others, rushing the body’s return to its pre-pregnancy state, or ignoring pain and discomfort can make recovery more difficult. Being patient with yourself and accepting this phase as a natural part of the journey into motherhood is key to moving through it with greater ease.
Finally, if at any point during the early postpartum period you experience unusual symptoms, severe pain, persistent emotional distress, or a sense of insecurity, consulting an obstetrician or gynecologist is the safest and most appropriate step. Caring for the mother is vital—not only for her own health, but also for the well-being of the newborn and the entire family.
If you are experiencing concerning symptoms in the early days after childbirth or feel that your recovery is not progressing as expected, a professional evaluation can provide reassurance and clarity.
If you wish, you may schedule a postpartum consultation and examination with Dr. Maryam Aghaei, Obstetrician and Gynecologist, to receive a thorough assessment of your physical and emotional health and personalized guidance tailored to your needs.




No comment