Breastfeeding and infant nutrition during the first months of life take up a significant amount of a mother’s time and energy. In the first two months after birth, newborns typically need 8 to 12 feeding sessions per day, and each feeding may last from a few minutes up to 30 minutes.
During this sensitive period, regular and adequate nutrition plays a crucial role in physical growth, brain development, and strengthening the infant’s immune system. Before birth, the baby received all essential nutrients through the mother’s body; after birth, healthy growth depends entirely on proper and sufficient feeding.
Mothers can choose one of several feeding methods based on their physical condition, emotional well-being, and lifestyle:
-
Breastfeeding with breast milk
-
Feeding with infant formula
-
A combination of breast milk and formula
Each method has its own benefits and limitations, and choosing the most appropriate option requires accurate information and informed decision-making.
In this article, we aim to provide a scientific, practical, and easy-to-understand guide on topics such as breastfeeding education, the benefits of breast milk, low milk supply, and choosing the most suitable feeding method, helping mothers make confident decisions for their baby’s health.
Feeding the Infant and Choosing the Right Nutrition
Feeding an infant is one of the most important responsibilities of parents during the early months of life. For healthy and natural growth, infants need a regular supply of fats, proteins, carbohydrates, vitamins, and minerals—nutrients that were previously supplied through the mother’s body during pregnancy and must now be provided through proper nutrition.

Adequate infant nutrition directly supports:
-
Brain and nervous system development
-
Bone and muscle growth
-
Proper function of vital organs
-
Strengthening of the immune system
Any deficiency or imbalance in nutrition may negatively affect the infant’s growth and development.
Mothers may choose one of the following feeding methods:
-
Breastfeeding with breast milk
-
Feeding with infant formula
-
Combination feeding (breast milk and formula)
From a scientific and medical perspective, most pediatricians and nutrition specialists consider breast milk to be the best nutritional option for infants.
Scientific Recommendations on the Duration of Breastfeeding

According to well-established scientific guidelines, infant feeding is recommended as follows:
-
First 6 months of life: Exclusive breastfeeding
-
Second 6 months: Continued breastfeeding along with age-appropriate complementary foods
This approach allows infants to receive maximum nutritional benefits during the most critical phase of growth. However, when breastfeeding is not possible, standard infant formula can adequately meet an infant’s nutritional needs.
Scientific Reasons for the Superiority of Breastfeeding
Breastfeeding is considered the optimal feeding method for infants due to multiple scientifically proven benefits. Breast milk contains biologically active components that are naturally designed for the infant’s body and support both short- and long-term health.

Key benefits of breast milk for infants include:
-
Strengthening the immune system and reducing the risk of infections
-
Lower incidence of colds, ear infections, diarrhea, and bacterial meningitis
-
Reduced risk of food allergies and digestive problems
-
Protection against Sudden Infant Death Syndrome (SIDS)
-
Reduced risk of insulin-dependent diabetes and certain chronic diseases
-
Improved cognitive development and higher average IQ
Studies show that breastfed infants are more likely to maintain a healthy weight later in life and are less prone to obesity or severe underweight.
According to the World Health Organization (WHO), exclusive breastfeeding for the first six months of life is the optimal feeding method. WHO also recommends initiating breastfeeding within the first hour after birth and continuing breastfeeding, alongside appropriate complementary foods, up to two years of age or beyond, as this promotes healthy growth, immune protection, and reduced disease risk.
Benefits of Breastfeeding for Mothers
The benefits of breastfeeding are not limited to infants; mothers also gain significant health advantages.
Benefits of breastfeeding for mothers include:
-
Faster uterine involution after childbirth
-
Increased calorie expenditure and easier return to pre-pregnancy weight
-
Reduced risk of breast cancer and some other cancers
-
Release of hormones that promote relaxation, reduce stress, and strengthen mother–infant bonding
-
Saving time and money by eliminating the need for formula and feeding equipment
Breastfeeding may also delay the return of menstruation; however, it should not be considered a reliable method of contraception.
Breastfeeding: A Significant and Challenging Responsibility
Despite its many benefits, breastfeeding is a major responsibility. Mothers who breastfeed are usually the primary caregivers responsible for feeding the infant at all hours, unless they express and store breast milk.
Returning to work, limited time for pumping, breast pain, or infections are common challenges some mothers face. While many mothers breastfeed without major difficulties, the experience is not the same for everyone.
Reasons for Choosing Formula Feeding
In certain situations, infant formula may be the most appropriate feeding option. Formula manufacturers continually improve formulations to make them nutritionally closer to breast milk.
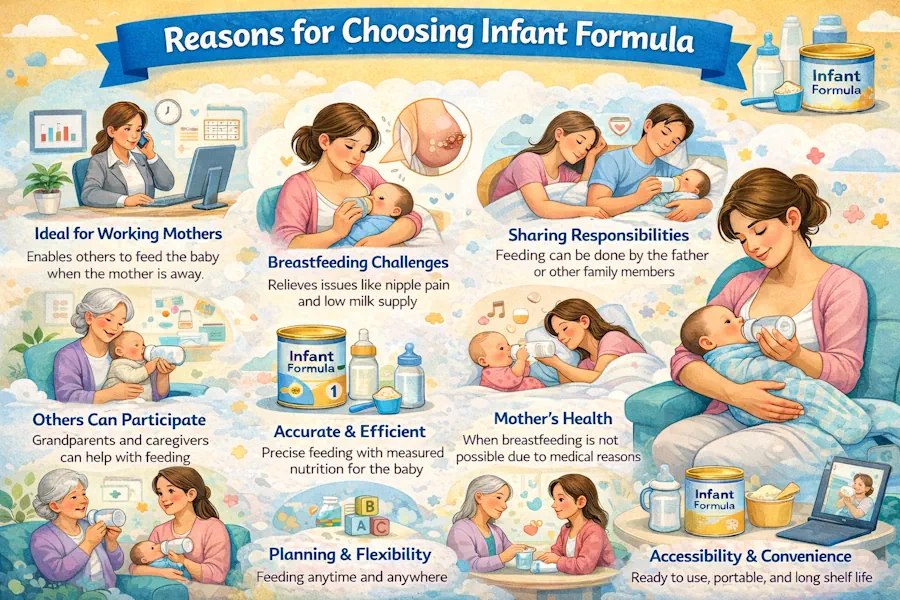
Common reasons for using infant formula include:
-
Maternal employment and lack of time for pumping breast milk
-
Ability to measure exact feeding volumes
-
Maternal preference not to breastfeed
-
Specific medical conditions in the mother or infant
Contrary to common misconceptions, most mothers are capable of producing enough milk, and the belief that “breast milk is not filling” is generally incorrect.
When mothers have specific medical conditions or require certain medications, formula feeding may be a safe and informed choice. In such cases, consultation with an obstetrician-gynecologist or pediatrician is essential.
Breast Milk or Formula? The Impact of Medical Conditions
The choice between breast milk and formula often depends on the medical condition of the mother or infant. While breast milk is usually the best option, in certain circumstances breastfeeding may be medically contraindicated, making formula feeding a safer alternative.
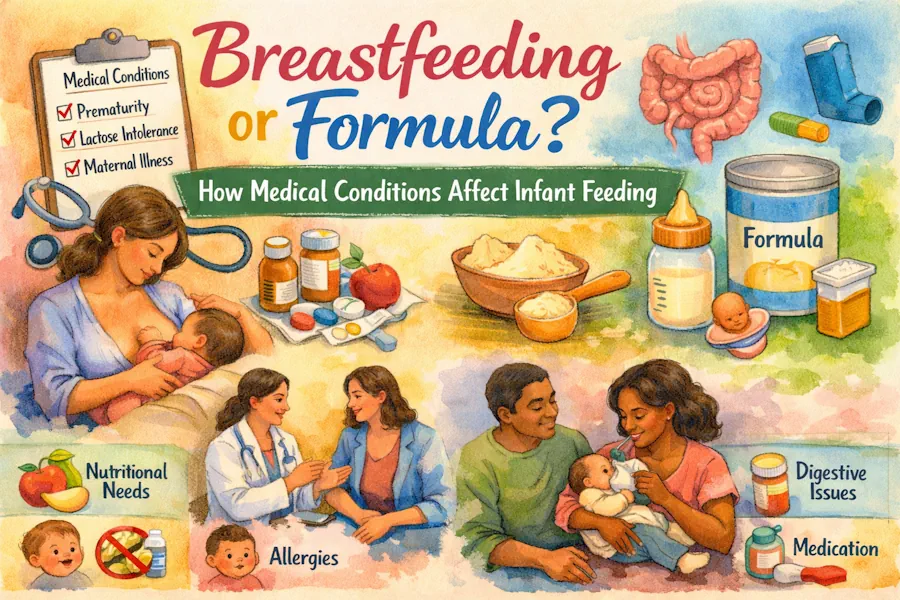
Understanding these conditions helps mothers make informed decisions without guilt or uncertainty.
When Should Breastfeeding Be Avoided?
Breastfeeding is generally contraindicated in the following situations:
-
Maternal HIV infection
-
Active, untreated tuberculosis
-
Ongoing cancer treatment (chemotherapy or radiotherapy)
-
Alcohol or illicit drug use
-
Use of medications harmful to the infant via breast milk
-
Infant galactosemia (a rare genetic carbohydrate metabolism disorder)
-
Infant phenylketonuria (PKU), a rare protein metabolism disorder
In these cases, specialized formula feeding under medical supervision is the safest option.
When Is Breastfeeding Possible Despite Medical Conditions?
Many medical conditions do not prevent breastfeeding. Breastfeeding may continue under medical guidance in the following situations:
-
Treatment of breast infections with breastfeeding-compatible antibiotics
-
Maternal hepatitis A, B, or C
-
Herpes infection (if no lesions are present on the breast and proper hygiene is maintained)
-
History of breast surgery
-
Infants with cleft lip or palate (if effective sucking is possible or with supportive techniques)
Final decisions should always be made in consultation with a pediatrician or obstetrician-gynecologist.
Principles of Formula Feeding

When breastfeeding is not possible or a mother chooses formula feeding, proper feeding principles are essential. The choice of formula, preparation method, and feeding equipment all influence infant health and comfort.
How to Suppress Breast Milk Production
After childbirth, hormonal changes stimulate milk production. If formula feeding is chosen, milk production should be gradually reduced to prevent pain, inflammation, or infection.
One commonly used method is applying cold cabbage leaves to the breasts.
How to use cabbage leaves:
-
Wash two large fresh cabbage leaves
-
Gently crush them to release juices
-
Place inside the bra over the breasts
-
Replace every 48 hours
Although the exact mechanism is unclear, cabbage leaves appear to have anti-inflammatory properties that reduce breast engorgement.
Important notes:
-
Breast size typically returns to normal within one to two weeks
-
Cold compresses or acetaminophen may help relieve pain
-
Avoid nipple stimulation, as it increases milk production
Choosing the Right Infant Formula
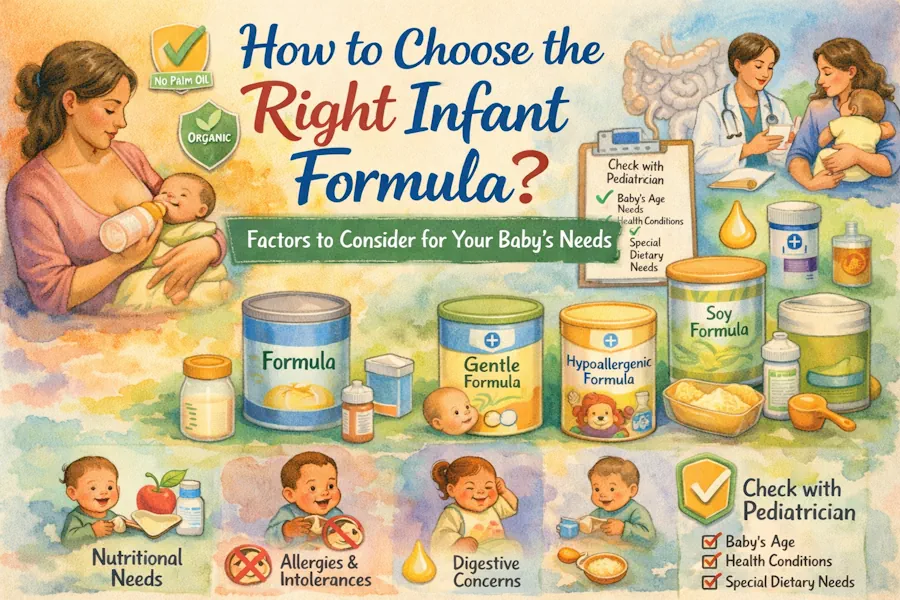
Infant formulas generally fall into several categories:
Cow’s Milk–Based Formula
-
Most commonly used
-
Modified to resemble human milk
-
Often recommended as the first choice by physicians
Soy-Based Formula
-
Suitable for infants with lactose intolerance or cow’s milk protein allergy
-
Symptoms of lactose intolerance include watery diarrhea, abdominal pain, and excessive crying
-
Should be used only under medical advice
Hydrolyzed (Protein-Broken) Formula
-
Least allergenic type
-
Proteins are broken down into amino acids
-
Suitable for infants with a family history of allergies
-
More expensive than standard formulas
Specialized Formulas
Designed for specific conditions such as:
-
Premature infants
-
Metabolic disorders
-
Severe digestive issues
These formulas should only be used with a physician’s prescription.
Forms of Infant Formula
Infant formulas are available in three forms:
-
Powdered (requires mixing with water)
-
Concentrated liquid
-
Ready-to-feed
Powdered formula is more economical but requires precise preparation. Some formulas are fortified with iron to prevent anemia. Others contain fatty acids such as DHA and ARA, which support brain development in breastfed infants, although their exact benefits in formula remain under study.
Signs of Formula Allergy in Infants
Contact a physician immediately if the infant shows:
-
Bloody diarrhea
-
Severe vomiting
-
Lethargy, weakness, or tremors
-
Skin rashes or persistent, unusual crying
Choosing the Right Bottle and Nipple
There is no single best bottle or nipple for all infants. Bottles are available in glass, plastic, and disposable types, while nipples vary in shape, material, and hole size.

Key points when choosing a bottle:
-
The best bottle is one the infant tolerates well
-
Trying different types may be necessary
-
Higher price does not necessarily mean better quality
Choosing the right nipple:
-
Always use age-appropriate nipples
-
Nipples designed for older infants have larger holes
-
Fast milk flow may cause choking, gas, or abdominal discomfort
If the infant experiences persistent gas or fussiness after feeding, changing the bottle or nipple may be helpful.
Frequently Asked Questions About Breastfeeding
How many times a day should an infant be fed?
Most infants require 8–12 feedings per day during the first months of life, with feeding intervals of 2–3 hours.
How long should each feeding last?
Each feeding typically lasts 10–30 minutes. Effective sucking and swallowing are more important than duration.
How can parents tell if an infant is getting enough milk?
Signs include appropriate weight gain, at least six wet diapers per day, calm behavior after feeding, and alertness.
What does low milk supply mean?
Low milk supply refers to insufficient milk intake, often due to ineffective latch, infrequent feeding, or maternal factors.
Does maternal stress affect breastfeeding?
Yes. Stress and fatigue can reduce milk-producing hormones. Adequate rest and emotional support are essential.
Can breast milk and formula be combined?
Yes. Combination feeding may be appropriate in certain situations, preferably under medical guidance.
Is breast pain normal during breastfeeding?
Mild discomfort is common initially, but severe pain, cracked nipples, or fever require medical evaluation.
Can all mothers breastfeed?
Most mothers can breastfeed, but certain medical conditions require professional assessment.
When should a doctor be consulted?
Seek medical advice for poor weight gain, abnormal sleepiness, reduced urination, persistent vomiting or diarrhea, or maternal breast infections.
Does breast milk lose its nutritional value over time?
No. Breast milk remains nutritious throughout the breastfeeding period and adapts to the infant’s needs.
Conclusion
Breastfeeding and infant nutrition play a vital role in a child’s physical growth, brain development, and long-term health. The early months of life are critical, and choosing the right feeding method can significantly reduce the risk of health complications.
Breast milk is scientifically recognized as the most complete form of nutrition for infants; however, medical conditions, lifestyle factors, or personal limitations may make formula or combination feeding a safe and reasonable choice. The most important factor is making an informed decision based on the infant’s needs, not societal pressure or misconceptions.
Concerns about low milk supply are common, but in most cases they can be managed with proper education, increased feeding frequency, correct latch techniques, and professional support. Monitoring infant cues, weight gain, and maintaining maternal well-being are key to successful feeding.
Ultimately, there is no single feeding method suitable for all mothers and infants. The best feeding choice is one that ensures the infant’s health while preserving the mother’s physical and emotional well-being. When in doubt, consulting a qualified obstetrician-gynecologist or pediatrician is the safest approach.



[…] Breast milk is the best option and supports immune system development […]
[…] six-week-old babies feed every 2 to 3 hours. Some babies may want to feed more frequently, which is normal, especially […]
[…] most cases, drastic dietary changes for the mother or discontinuing breastfeeding do not improve colic. Medications or home remedies should not be used without medical […]
[…] the fourth week of life, Breastfeeding remains central to the baby’s growth and health. A 4-week-old baby is usually fed exclusively […]
[…] possible, breast milk is the best option and meets all nutritional needs. However, babies fed with formula can also grow […]
[…] milk is the best and most complete source of nutrition at this age. If breastfeeding is not possible, formula feeding should be done under medical […]
[…] a process accompanied by uterine contractions. These contractions often become stronger during breastfeeding due to increased release of the hormone oxytocin.The pain is usually similar to menstrual cramps […]