Vaginal dryness is one of the common problems among women that can occur at any age and may cause symptoms such as burning, itching, pain during sexual intercourse, and decreased sexual desire. This condition most commonly occurs due to a decrease in the hormone estrogen; however, other factors such as stress, the use of certain medications, breastfeeding, menopause, or even insufficient sexual stimulation can also play a role in its development. In this article, we will discuss what vaginal dryness is.
Many individuals who experience these symptoms become concerned and ask questions such as:
What is vaginal dryness a sign of? Is vaginal dryness dangerous? And most importantly, how is vaginal dryness treated?
The good news is that in most cases, vaginal dryness is treatable. By identifying the underlying cause, it is possible to use simple home remedies as well as medical and pharmacological treatments to improve this condition. In this article, we comprehensively examine what vaginal dryness is, what symptoms it causes, why it occurs, and what the best treatment options are, so that you can make informed and confident decisions about your health.
What Is Vaginal Dryness?
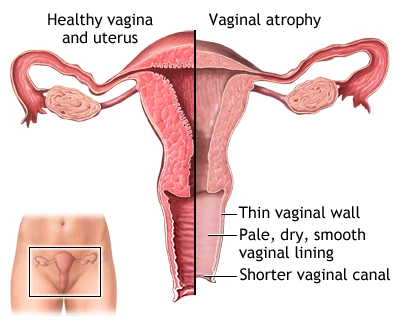
Vaginal dryness is a condition in which the internal tissues of the vagina lose their natural moisture, softness, and elasticity. Under normal circumstances, the vaginal walls are lubricated by natural secretions that help prevent irritation, pain, and injury. When these secretions decrease, the vagina becomes dry, thin, and sensitive, which can cause discomfort during daily activities or sexual intercourse.
This condition most commonly occurs due to a reduction in estrogen levels. Estrogen plays a crucial role in maintaining the health of vaginal tissues. When estrogen levels decline, blood flow and vaginal moisture decrease as well. For this reason, vaginal dryness is more common during menopause; however, it is not limited to menopause and can also occur in younger women, during breastfeeding, or as a result of certain medications.
Vaginal dryness is not considered a dangerous disease, but if left untreated, it can negatively affect quality of life, sexual relationships, and emotional well-being. Fortunately, by identifying the underlying cause, there are many effective treatment options available.
What Is Vaginal Dryness Called in English?
The term “vaginal dryness” in English is Vaginal Dryness. In medical literature, this condition may also be discussed as part of Vaginal Atrophy or Genitourinary Syndrome of Menopause (GSM), particularly in postmenopausal women.
What Is Uterine Dryness? Is It Different from Vaginal Dryness?

The term “uterine dryness” is commonly used among Persian-speaking individuals; however, from a medical perspective, it is not an accurate term. In most cases, when people refer to uterine dryness, they are actually describing vaginal dryness.
The uterus is an internal organ and does not directly become dry. Symptoms such as burning, pain during sexual intercourse, or a sensation of dryness are typically related to the vagina or the vulvar area, not the uterus itself. For this reason, medical and scientific sources use the term “vaginal dryness.”
If you experience dryness, burning, or pain, it is most likely related to vaginal dryness, and a medical evaluation can help determine the exact cause.
Is Vaginal Dryness Common and Who Is More Likely to Be Affected?
Vaginal dryness is a relatively common condition, and many individuals experience it at some point in their lives. The belief that vaginal dryness only occurs during menopause is incorrect. Although it is more prevalent after menopause, it can also occur at younger ages.
Studies indicate that approximately 15–20% of women aged 18 to 50 experience vaginal dryness, particularly during sexual intercourse. After menopause, due to a significant decline in estrogen levels, more than half of postmenopausal women experience vaginal dryness. As a result, it is considered one of the most common physical changes associated with menopause.
Groups that are more likely to experience vaginal dryness include:
-
Women during and after menopause
-
Women who are breastfeeding or have recently given birth
-
Younger women who use oral contraceptives or hormonal medications
-
Individuals undergoing cancer treatments such as chemotherapy or hormone therapy
-
People with certain medical conditions such as diabetes or autoimmune disorders
-
Individuals who frequently use scented soaps, gels, or cleansers in the genital area
In many cases, vaginal dryness is a natural and manageable condition and is not necessarily a sign of a serious disease. Awareness of its prevalence and contributing factors is the first step toward choosing appropriate treatment and preventing symptom progression.
What Are the Symptoms of Vaginal Dryness?

The symptoms of vaginal dryness can range from mild to severe and vary from person to person. Some individuals only notice symptoms during sexual intercourse, while others may experience discomfort during everyday activities. Recognizing these symptoms helps with early diagnosis and effective treatment.
Common symptoms of vaginal dryness include:
-
A feeling of dryness, burning, or itching inside or around the vagina
-
Pain or discomfort during sexual intercourse, especially during penetration
-
A burning sensation during urination
-
Decreased sexual desire due to pain or discomfort
-
Mild bleeding after intercourse caused by thinning of the vaginal walls
-
A sensation of tightness or pain in the vulvar area (external genital area)
-
Recurrent urinary tract or vaginal yeast infections
In more severe cases, individuals may experience burning or discomfort even while walking, sitting for long periods, or wearing tight underwear. This can significantly affect quality of life, self-confidence, and emotional relationships.
If these symptoms persist or do not improve with simple home treatments, consulting a gynecologist is recommended to determine the underlying cause and appropriate treatment.
What Causes Vaginal Dryness?

In most cases, vaginal dryness is caused by a decrease in estrogen levels. Estrogen plays a vital role in maintaining vaginal moisture, thickness, and elasticity. When estrogen levels decline, the vaginal walls become thinner and natural lubrication decreases, resulting in vaginal dryness.
Although reduced estrogen is the most common cause, it is not the only factor. The main causes of vaginal dryness include:
Decreased Estrogen Levels
This is the most common cause and typically occurs in the following situations:
-
Menopause and postmenopause
-
Breastfeeding and the postpartum period
-
Surgical removal of the ovaries
-
Chemotherapy or hormone therapy
Certain Medications
Some medications can reduce vaginal moisture, including:
-
Oral contraceptives and hormonal medications
-
Antidepressants
-
Antihistamines
-
Anti-estrogen medications used for conditions such as endometriosis or fibroids
Causes of Vaginal Dryness in Younger Women
Vaginal dryness is not limited to older age. In younger women, it may be caused by:
-
Severe stress or anxiety
-
Insufficient sexual stimulation or inadequate foreplay
-
Temporary hormonal changes
-
Frequent use of scented soaps and cleansers
Medical Conditions
Certain medical conditions can contribute to vaginal dryness, including:
-
Diabetes
-
Sjögren’s syndrome (an autoimmune disorder)
-
Hormonal disorders
Lifestyle and Environmental Factors
-
Excessive vaginal washing
-
Use of vaginal sprays, gels, or douching
-
Smoking
-
Dehydration
Vaginal dryness is often caused by a combination of factors. Identifying the exact cause plays a key role in selecting the most effective treatment. If symptoms persist, medical evaluation is recommended.
What Causes Vaginal Dryness in Younger Women?

Vaginal dryness is not exclusive to menopause and can also affect younger women. In this age group, non-menopausal factors are usually responsible.
The most common causes include:
-
Stress, anxiety, and psychological pressure
-
Use of oral contraceptives or hormonal medications
-
Insufficient sexual stimulation or foreplay
-
Temporary hormonal fluctuations
-
Frequent use of scented soaps and cleansers
-
Breastfeeding or the postpartum period
In many cases, vaginal dryness in younger women can be effectively managed through lifestyle adjustments and appropriate treatment.
What Is Vaginal Dryness a Sign Of?
Vaginal dryness is usually a sign of hormonal changes or the body’s response to specific conditions and does not typically indicate a serious illness. The most common underlying factor is reduced estrogen levels.
Vaginal dryness may indicate:
-
The onset of menopause or perimenopause
-
Breastfeeding or postpartum hormonal changes
-
Use of certain medications
-
Severe stress or chronic fatigue
-
Insufficient sexual stimulation
However, if vaginal dryness appears suddenly, becomes severe, or is accompanied by unusual symptoms, medical evaluation is recommended to rule out other conditions.
Is Vaginal Dryness Dangerous?

In most cases, vaginal dryness itself is not dangerous and is not considered a serious medical condition. It is often caused by hormonal changes, particularly reduced estrogen levels, and can usually be managed with simple treatments.
However, if left untreated or if it persists long-term, vaginal dryness can lead to complications that affect quality of life, including:
-
Severe pain during sexual intercourse and avoidance of intimacy
-
Decreased sexual desire and emotional distance from a partner
-
Increased risk of recurrent vaginal and urinary tract infections
-
Cracks, inflammation, or mild bleeding of the vaginal walls
In rare cases, vaginal dryness may indicate an underlying condition such as hormonal disorders, autoimmune diseases, or medication side effects. Medical evaluation is essential if symptoms include abnormal bleeding, severe pain, persistent burning, or lack of response to basic treatments.
Overall, vaginal dryness is a common and treatable condition, and early diagnosis helps prevent potential complications.
Is Vaginal Dryness a Sign of Pregnancy?
Vaginal dryness is not typically a direct sign of pregnancy. In early pregnancy, hormonal changes usually lead to increased vaginal discharge rather than dryness.
In rare cases, hormonal fluctuations, stress, or dehydration during pregnancy may cause a sensation of dryness. Therefore, vaginal dryness alone is not a reliable indicator of pregnancy.
To confirm pregnancy, attention to other symptoms and performing a pregnancy test are necessary.
How Is Vaginal Dryness Diagnosed?

Vaginal dryness is usually diagnosed by a gynecologist based on symptoms, medical history, and physical examination. In many cases, describing the experienced symptoms plays a key role in accurate diagnosis.
The physician may ask about:
-
Severity and duration of vaginal dryness symptoms
-
Presence of pain during intercourse or burning and itching
-
Menstrual status, menopause, or breastfeeding
-
Medications currently being used
If necessary, the following diagnostic methods may be used:
-
Pelvic examination: To assess the vaginal walls for dryness, thinning, or inflammation
-
Blood tests: To evaluate hormone levels, especially estrogen, or identify hormonal disorders
-
Vaginal discharge testing: To rule out bacterial or fungal infections with similar symptoms
Accurate diagnosis is essential, as treatment depends on the underlying cause. Prolonged self-treatment without medical evaluation is not recommended, especially if symptoms are severe or persistent.
How Is Vaginal Dryness Treated?

Treatment for vaginal dryness depends on the underlying cause, severity of symptoms, and the individual’s physical condition. In many cases, simple and non-invasive methods are effective, while others may require medical or pharmacological treatment.
The primary goals of treatment are to increase vaginal moisture, reduce pain and burning, and improve quality of life and sexual comfort. Fortunately, a wide range of treatment options is available.
Below are the most effective treatments for vaginal dryness.
What Medications Are Used for Vaginal Dryness and When Are They Prescribed?
When vaginal dryness is caused by reduced estrogen levels, medical treatment can be highly effective. These medications work by replacing or mimicking estrogen and are available only by prescription.
Common medications include:
-
Low-dose vaginal estrogen creams, tablets, or suppositories
-
Vaginal estrogen rings that remain in place for several months
-
Oral medications such as Ospemifene
-
Vaginal DHEA for reducing pain during intercourse in postmenopausal women
⚠️ Note: Estrogen-based treatments are not suitable for everyone, especially individuals with a history of breast cancer or certain medical conditions. These medications must be used under medical supervision.
Non-Medication Treatments for Vaginal Dryness
For mild to moderate cases, or when medication is not recommended, non-pharmacological methods may be helpful:
-
Vaginal moisturizers used every few days to maintain natural moisture
-
Vaginal lubricants, especially before intercourse, to reduce friction and pain
-
Increased sexual stimulation and adequate foreplay
-
Avoidance of scented soaps and cleansers in the genital area
These methods are generally safe and are often considered first-line treatments.
Treatment of Vaginal Dryness During Menopause
During menopause, vaginal dryness is more common and may be more severe due to a significant drop in estrogen levels. In such cases, a combination of:
-
Local estrogen therapy
-
Vaginal moisturizers and lubricants
-
In some cases, advanced medical treatments
may provide the best results. Treatment should be individualized based on medical advice.
Medical and Clinical Treatments for Vaginal Dryness

When vaginal dryness is severe or does not respond to conventional treatments, certain clinical procedures, such as energy-based devices (e.g., vaginal radiofrequency), may be recommended. These treatments must be performed by qualified specialists in reputable medical centers and are not suitable for everyone.
Vaginal dryness is a treatable condition, and with appropriate management, symptoms often improve significantly. If symptoms are severe, persistent, or accompanied by pain or bleeding, medical consultation is essential.
What Are Home Remedies?

Home remedies are usually effective for mild to moderate cases and can help reduce burning, itching, and discomfort. They are often safe and can be used as first-line treatment or alongside medical therapy.
Common home remedies include:
Vaginal Lubricants and Moisturizers
-
Vaginal moisturizers help maintain moisture when used every few days
-
Vaginal lubricants are typically used before intercourse to reduce friction and pain
🔹 Recommendation: Water-based lubricants are the safest option, especially when using condoms.
Natural Oils
Some natural oils may be used externally as lubricants, including:
-
Coconut oil
-
Olive oil
-
Grapeseed oil
-
Sunflower oil
These oils should only be used externally and before intercourse. Note that oil-based products can damage condoms and are not suitable for pregnancy prevention.
Increasing Sexual Stimulation and Foreplay
Natural vaginal lubrication is closely linked to sexual arousal. Spending more time on foreplay, reducing stress, and improving communication with a partner can enhance natural lubrication.
Staying Hydrated
Dehydration can reduce moisture throughout the body, including vaginal tissues. Drinking adequate water helps maintain proper hydration.
Avoiding Irritants
To prevent worsening:
-
Avoid scented soaps and cleansers
-
Do not perform vaginal douching
-
Wear loose, cotton underwear
While home remedies may relieve symptoms, medical evaluation is recommended if vaginal dryness is severe, persistent, or accompanied by pain or bleeding.
Treatment During Sexual Intercourse

Vaginal dryness during sexual intercourse is one of the most common causes of pain during penetration (dyspareunia). Insufficient lubrication increases friction, leading to burning, pain, and sometimes mild bleeding. This unpleasant experience may eventually reduce sexual desire and lead to avoidance of intimacy.
To reduce dryness and pain during intercourse, the following measures can be helpful:
Use of Appropriate Lubricants
Applying water-based or silicone-based vaginal lubricants before intercourse is one of the simplest and most effective ways to reduce dryness and pain.
Increased Foreplay and Sexual Stimulation
Adequate arousal is essential for natural vaginal lubrication. Spending sufficient time on foreplay can significantly improve comfort.
Reducing Stress and Anxiety
Stress, fear of pain, or anxiety can cause vaginal muscle tension and reduce arousal. Open communication with a partner and creating a relaxed environment are important.
Choosing Comfortable Sexual Positions
Some positions allow better control of penetration depth and speed, reducing discomfort.
Regular Use of Vaginal Moisturizers
Using vaginal moisturizers regularly, not only during intercourse, can improve overall vaginal hydration.
If vaginal dryness during intercourse persists despite these measures, medical evaluation and treatment may be necessary.
When Should You See a Doctor?

In many cases, vaginal dryness can be managed with home remedies or simple treatments. However, medical consultation is recommended in the following situations:
-
Severe or persistent vaginal dryness that does not improve with over-the-counter treatments
-
Significant pain during intercourse or bleeding afterward
-
Interference with daily activities or quality of life
-
Associated symptoms such as severe burning, persistent itching, or abnormal discharge
-
History of early menopause, hormonal disorders, or autoimmune diseases
-
Use of medications known to cause vaginal dryness
A physician can identify the underlying cause and recommend appropriate treatment, helping prevent symptom progression and complications.
Frequently Asked Questions (FAQ)
What is vaginal dryness?
Vaginal dryness occurs when vaginal tissues lose their natural moisture, leading to symptoms such as burning, itching, or pain during intercourse, often due to decreased estrogen levels.
What causes vaginal dryness?
The most common cause is reduced estrogen, but menopause, breastfeeding, medications, stress, insufficient sexual stimulation, and inappropriate hygiene products can also contribute.
Is vaginal dryness dangerous?
It is usually not dangerous, but untreated dryness can cause pain, infections, and reduced quality of life. Medical evaluation is recommended if symptoms persist.
What are the symptoms of vaginal dryness?
Symptoms include dryness, burning, itching, pain during intercourse, mild post-intercourse bleeding, and burning during urination.
Does vaginal dryness occur in younger women?
Yes. It can occur in younger women due to stress, hormonal contraceptives, hormonal changes, breastfeeding, or insufficient sexual stimulation.
What are home remedies for vaginal dryness?
Home remedies include vaginal lubricants and moisturizers, adequate hydration, avoiding scented products, and increasing foreplay.
What medications are used for vaginal dryness?
Doctors may prescribe vaginal estrogen, oral medications like ospemifene, or vaginal DHEA. These should be used under medical supervision.
How is vaginal dryness during intercourse treated?
Using water-based lubricants, increasing foreplay, reducing stress, and using vaginal moisturizers regularly can help.
Is vaginal dryness a sign of pregnancy?
Vaginal dryness is not typically a sign of pregnancy. Hormonal changes in pregnancy usually increase vaginal discharge.
When should I see a doctor?
If dryness is severe, persistent, associated with pain, bleeding, infections, or does not improve with home remedies, medical consultation is advised.
Summary and Medical Advice
Vaginal dryness is a common and treatable condition that can occur at any age due to hormonal changes, menopause, breastfeeding, medication use, or lifestyle factors. Although it is usually not dangerous, neglecting it can lead to pain during intercourse, reduced sexual desire, and decreased quality of life.
Early identification of the underlying cause and appropriate treatment selection play a crucial role in symptom improvement. In many cases, vaginal moisturizers, lubricants, and simple lifestyle adjustments are effective, while more severe cases may require medical treatment under physician supervision.
Medical Recommendation:
If your vaginal dryness is persistent, associated with pain or bleeding, or does not improve with home remedies, consult a gynecologist without hesitation. In most cases, this condition is manageable, and proper treatment can significantly improve physical health, emotional well-being, and sexual quality of life.
Vaginal dryness is a solvable condition. If your symptoms persist or affect your quality of life, consulting a specialist can help determine the most appropriate treatment plan.


No comment